| Title |
Determining Risk of Barrett’s Esophagus and Esophageal Adenocarcinoma Based on Epidemiologic Factors and Genetic Variants
|
|---|---|
| Published in |
Gastroenterology, December 2017
|
| DOI | 10.1053/j.gastro.2017.12.003 |
| Pubmed ID | |
| Authors |
Jing Dong, Matthew F. Buas, Puya Gharahkhani, Bradley J. Kendall, Lynn Onstad, Shanshan Zhao, Lesley A. Anderson, Anna H. Wu, Weimin Ye, Nigel C. Bird, Leslie Bernstein, Wong-Ho Chow, Marilie D. Gammon, Geoffrey Liu, Carlos Caldas, Paul D. Pharoah, Harvey A. Risch, Prasad G. Iyer, Brian J. Reid, Laura J. Hardie, Jesper Lagergren, Nicholas J. Shaheen, Douglas A. Corley, Rebecca C. Fitzgerald, Stomach and Oesophageal Cancer Study consortium, David C. Whiteman, Thomas L. Vaughan, Aaron P. Thrift |
| Abstract |
We developed comprehensive models to determine risk of Barrett's esophagus (BE) or esophageal adenocarcinoma (EAC) based on genetic and non-genetic factors. We used pooled data from 3288 patients with BE, 2511 patients with EAC, and 2177 individuals without either (controls) from participants in the international Barrett's and EAC consortium as well as the United Kingdom's BE gene study and stomach and esophageal cancer study. We collected data on 23 genetic variants associated with risk for BE or EAC, and constructed a polygenic risk score (PRS) for cases and controls by summing the risk allele counts for the variants weighted by their natural log-transformed effect estimates (odds ratios) extracted from genome-wide association studies. We also collected data on demographic and lifestyle factors (age, sex, smoking, body mass index, use of nonsteroidal anti-inflammatory drugs) and symptoms of gastroesophageal reflux disease (GERD). Risk models with various combinations of non-genetic factors and the PRS were compared for their accuracy in identifying patients with BE or EAC using the area under the receiver operating characteristic curve (AUC) analysis. Individuals in the highest quartile of risk, based on genetic factors (PRS), had a 2-fold higher risk of BE (odds ratio, 2.22; 95% confidence interval, 1.89-2.60) or EAC (odds ratio, 2.46; 95% confidence interval, 2.07-2.92) than individual in the lowest quartile of risk based on PRS. Risk models developed based on only demographic or lifestyle factors or GERD symptoms identified patients with BE or EAC with AUC values ranging from 0.637 to 0.667. Combining data on demographic or lifestyle factors with data on GERD symptoms identified patients with BE with an AUC of 0.793 and patients with EAC with an AUC of 0.745. Including PRSs with these data only minimally increased the AUC values for BE (to 0.799) and EAC (to 0.754). Including the PRSs in the model developed based on non-genetic factors resulted in a net reclassification improvement for BE of 3.0% and for EAC of 5.6%. We used data from 3 large databases of patients from studies of BE or EAC to develop a risk prediction model based on genetic, clinical, and demographic/lifestyle factors. We identified a PRS that increases discrimination and net reclassification of individuals with vs without BE and EAC. However, the absolute magnitude of improvement is not sufficient to justify its clinical use. |
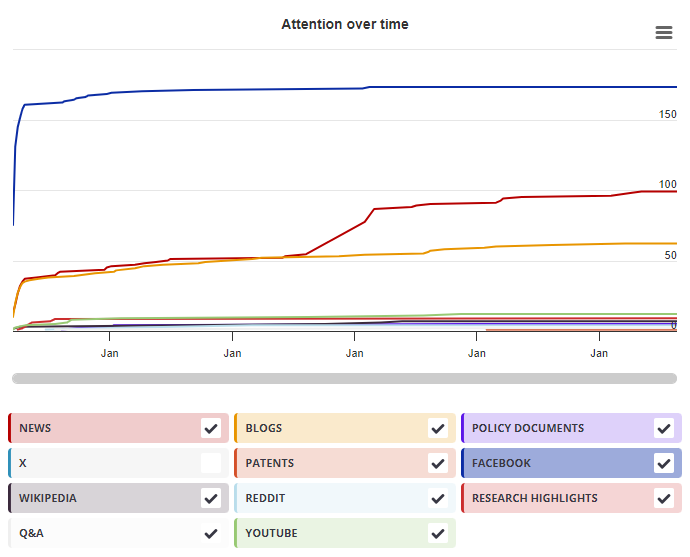
X Demographics
As of 1 July 2024, you may notice a temporary increase in the numbers of X profiles with Unknown location. Click here to learn more.
Geographical breakdown
| Country | Count | As % |
|---|---|---|
| United Kingdom | 5 | 31% |
| United States | 2 | 13% |
| Germany | 1 | 6% |
| France | 1 | 6% |
| Unknown | 7 | 44% |
Demographic breakdown
| Type | Count | As % |
|---|---|---|
| Members of the public | 7 | 44% |
| Scientists | 4 | 25% |
| Practitioners (doctors, other healthcare professionals) | 3 | 19% |
| Science communicators (journalists, bloggers, editors) | 2 | 13% |
Mendeley readers
Geographical breakdown
| Country | Count | As % |
|---|---|---|
| Unknown | 90 | 100% |
Demographic breakdown
| Readers by professional status | Count | As % |
|---|---|---|
| Student > Ph. D. Student | 13 | 14% |
| Researcher | 9 | 10% |
| Student > Bachelor | 8 | 9% |
| Student > Master | 6 | 7% |
| Other | 6 | 7% |
| Other | 19 | 21% |
| Unknown | 29 | 32% |
| Readers by discipline | Count | As % |
|---|---|---|
| Medicine and Dentistry | 26 | 29% |
| Biochemistry, Genetics and Molecular Biology | 7 | 8% |
| Agricultural and Biological Sciences | 3 | 3% |
| Nursing and Health Professions | 3 | 3% |
| Pharmacology, Toxicology and Pharmaceutical Science | 2 | 2% |
| Other | 8 | 9% |
| Unknown | 41 | 46% |